The NEJM has an article an editorial on CT screening for lung cancer. The article notes:
The rate of adherence to screening was more than 90%. The rate of positive screening tests was 24.2% with low-dose CT and 6.9% with radiography over all three rounds. A total of 96.4% of the positive screening results in the low-dose CT group and 94.5% in the radiography group were false positive results. The incidence of lung cancer was 645 cases per 100,000 person-years (1060 cancers) in the low-dose CT group, as compared with 572 cases per 100,000 person-years (941 cancers) in the radiography group
The rate of death was reduced by 6.7%.
The editorial noted:
The NLST results show that three annual rounds of low-dose CT screening reduce mortality from lung cancer, and that the rate of death associated with diagnostic procedures is low.
And:
According to the authors, 7 million U.S. adults meet the entry criteria for the NLST,1 and an estimated 94 million U.S. adults are current or former smokers. With either target population, a national screening program of annual low-dose CT would be very expensive, which is why I agree with the authors that policy makers should wait for more information before endorsing lung-cancer screening programs.
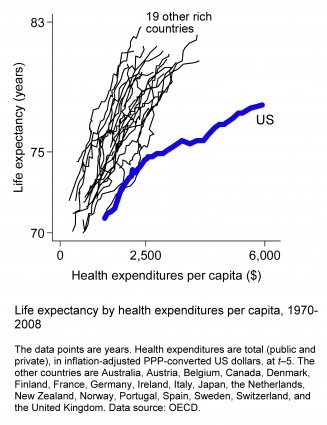
Medicynical Note: This screening is quite costly even without considering the costs of sorting out the false positives. There is a question whether any system of care, much less one that is bankrupting a nation, can afford such a screening program. Would, for example, some of the funds be better employed in education about the hazards of smoking and smoking cessation.